Link:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10200714/
Graphic:
Excerpt:
Background
Persistent multi-organ symptoms after COVID-19 have been termed “long COVID” or “post-acute sequelae of SARS-CoV-2 infection” (PASC). The complexity of these clinical manifestations posed challenges early in the pandemic as different ambulatory models formed out of necessity to manage the influx of patients. Little is known about the characteristics and outcomes of patients seeking care at multidisciplinary post-COVID centers.
Methods
We performed a retrospective cohort study of patients evaluated at our multidisciplinary Comprehensive COVID-19 Center (CCC) in Chicago, IL, between May 2020 and February 2022. We analyzed specialty clinic utilization and clinical test results according to severity of acute COVID-19.
Results
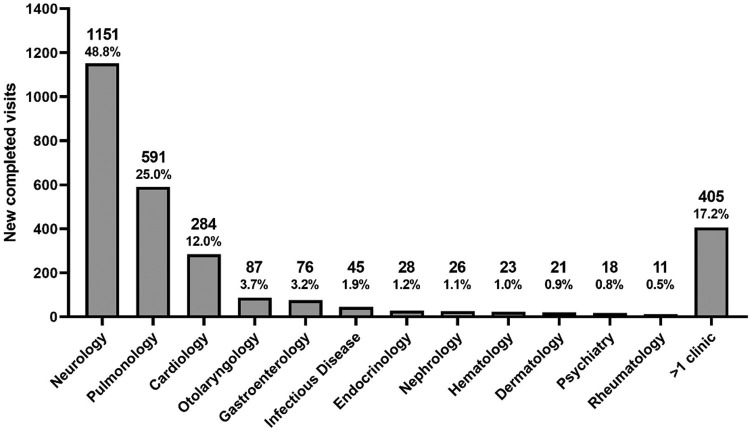
We evaluated 1802 patients a median of 8 months from acute COVID-19 onset, including 350 post-hospitalization and 1452 non-hospitalized patients. Patients were seen in 2361 initial visits in 12 specialty clinics, with 1151 (48.8%) in neurology, 591 (25%) in pulmonology, and 284 (12%) in cardiology. Among patients tested, 742/878(85%) reported decreased quality of life, 284/553(51%) had cognitive impairment, 195/434(44.9%) had alteration of lung function, 249/299(83.3%) had abnormal CT chest scans, and 14/116(12.1%) had elevated heart rate on rhythm monitoring. Frequency of cognitive impairment and pulmonary dysfunction was associated with severity of acute COVID-19. Non-hospitalized patients with positive SARS-CoV-2 testing had similar findings than those with negative or no test results.
Conclusions
The CCC experience shows common utilization of multiple specialists by long COVID patients, who harbor frequent neurologic, pulmonary, and cardiologic abnormalities. Differences in post-hospitalization and non-hospitalized groups suggest distinct pathogenic mechanisms of long COVID in these populations.
Keywords: Long COVID, Post-Acute Sequelae of SARS-CoV-2 Infection, PASC, Multidisciplinary Care, Health Service Delivery
doi: 10.1016/j.amjmed.2023.05.002 [Epub ahead of print]
Author(s): Joseph Bailey, M.D.,a,⁎ Bianca Lavelle, M.D.,b Janet Miller, B.S.,a Millenia Jimenez, B.S.,c Patrick H. Lim, M.S.,c Zachary S. Orban, B.S.,c Jeffrey R. Clark, B.A.,c Ria Tomar, B.S.,a Amy Ludwig, M.D.,a Sareen T. Ali, B.S.,c Grace K. Lank, B.S.,c Allison Zielinski, M.D.,d Ruben Mylvaganam, M.D.,a Ravi Kalhan, M.D.,a Malek El Muayed, M.D.,e R. Kannan Mutharasan, M.D.,d Eric M. Liotta, M.D. M.S.,c Jacob I Sznajder, M.D.,a Charles Davidson, M.D.,d Igor J. Koralnik, M.D.,c,1 and Marc A. Sala, M.D.a,1, for the Northwestern Medicine Comprehensive COVID Center Investigators
Publication Date: 2023 May 22
Publication Site: National Library of Medicine