Link: https://www.nature.com/articles/s41598-021-83040-3
Graphic:
Abstract:
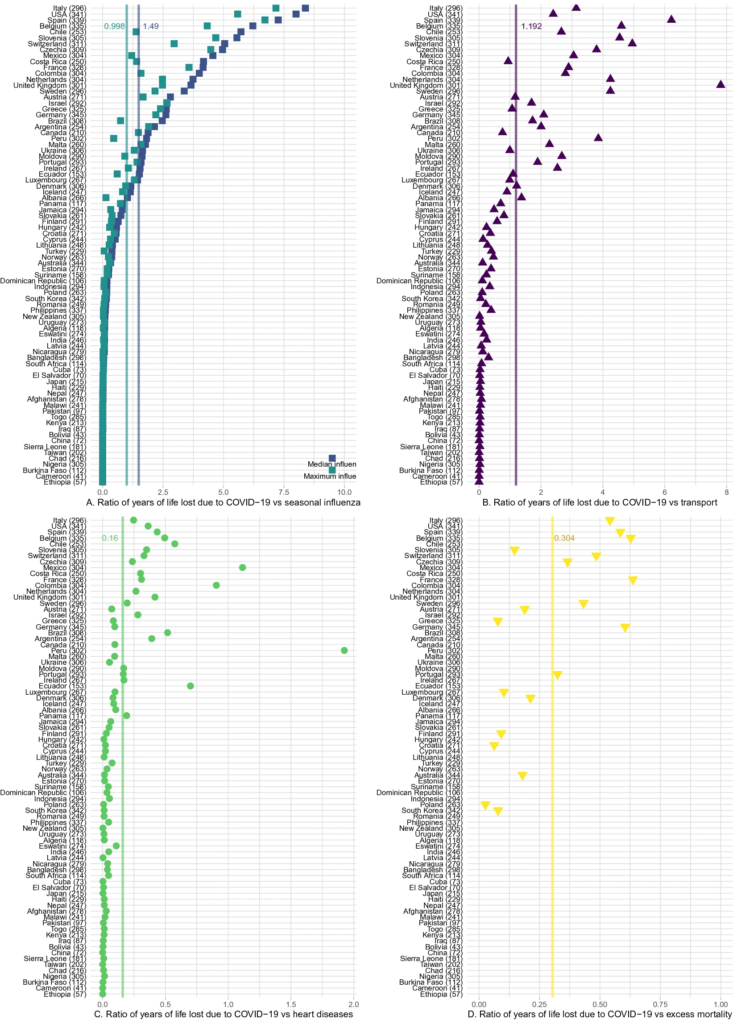
Understanding the mortality impact of COVID-19 requires not only counting the dead, but analyzing how premature the deaths are. We calculate years of life lost (YLL) across 81 countries due to COVID-19 attributable deaths, and also conduct an analysis based on estimated excess deaths. We find that over 20.5 million years of life have been lost to COVID-19 globally. As of January 6, 2021, YLL in heavily affected countries are 2–9 times the average seasonal influenza; three quarters of the YLL result from deaths in ages below 75 and almost a third from deaths below 55; and men have lost 45% more life years than women. The results confirm the large mortality impact of COVID-19 among the elderly. They also call for heightened awareness in devising policies that protect vulnerable demographics losing the largest number of life-years.
Author(s): Héctor Pifarré i Arolas, Enrique Acosta, Guillem López-Casasnovas, Adeline Lo, Catia Nicodemo, Tim Riffe & Mikko Myrskylä
Publication Date: 18 Feb 2021
Publication Site: nature scientific reports