Link: https://content.govdelivery.com/accounts/FLDOH/bulletins/3312697
Graphic:
Excerpt:
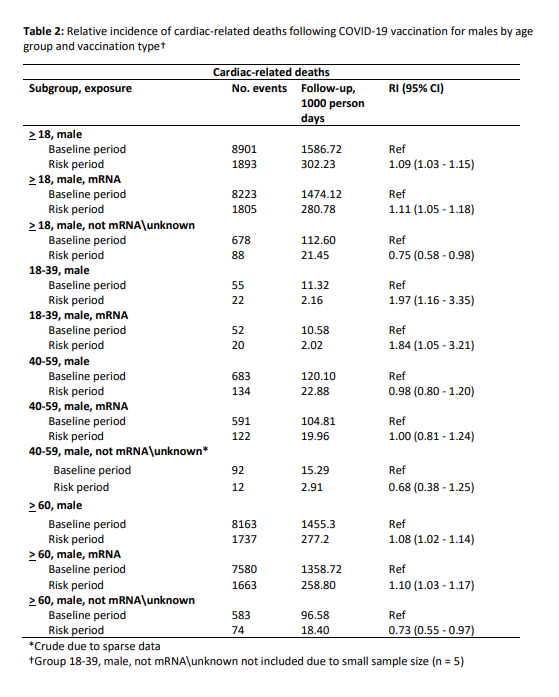
Today, State Surgeon General Dr. Joseph A. Ladapo has announced new guidance regarding mRNA vaccines. The Florida Department of Health (Department) conducted an analysis through a self-controlled case series, which is a technique originally developed to evaluate vaccine safety.
This analysis found that there is an 84% increase in the relative incidence of cardiac-related death among males 18-39 years old within 28 days following mRNA vaccination. With a high level of global immunity to COVID-19, the benefit of vaccination is likely outweighed by this abnormally high risk of cardiac-related death among men in this age group. Non-mRNA vaccines were not found to have these increased risks.
As such, the State Surgeon General recommends against males aged 18 to 39 from receiving mRNA COVID-19 vaccines. Those with preexisting cardiac conditions, such as myocarditis and pericarditis, should take particular caution when making this decision.
Author(s): Joseph A. Ladapo
Publication Date: 7 Oct 2022
Publication Site: Florida Dept of Health