Graphic:
Excerpt:
Making those timelines — 2020, 2021, 2022, 2023, 2024 — really brought home to me how long this pandemic has been going on; I lost track in the daily grind (though the daily grind is also my form of coping). And it’s a bit discouraging to see the most solidarity our society seems capable of fizzle out after 2020, followed by a struggle to return to business as usual, a struggle that failed by 2024, in that a once-essential part of touring — contact with the fans — has now gone missing.
We can, of course, moralize about what how these artists have gone about their business:
To be fair, though, when CDC Director Mandy Cohen is swanning about with no mask, modeling how to infect everybody she breathes on, what’s a poor celebrity to do? Restoring social norms that support non-pharmaceutical interventions will probably take a whole-of-society approach (which could happen when those Tiktokers start doing their research).
Here, however, are two small steps artists like Adele and Taylor Swift could do to improve the Covid pandemic situation.
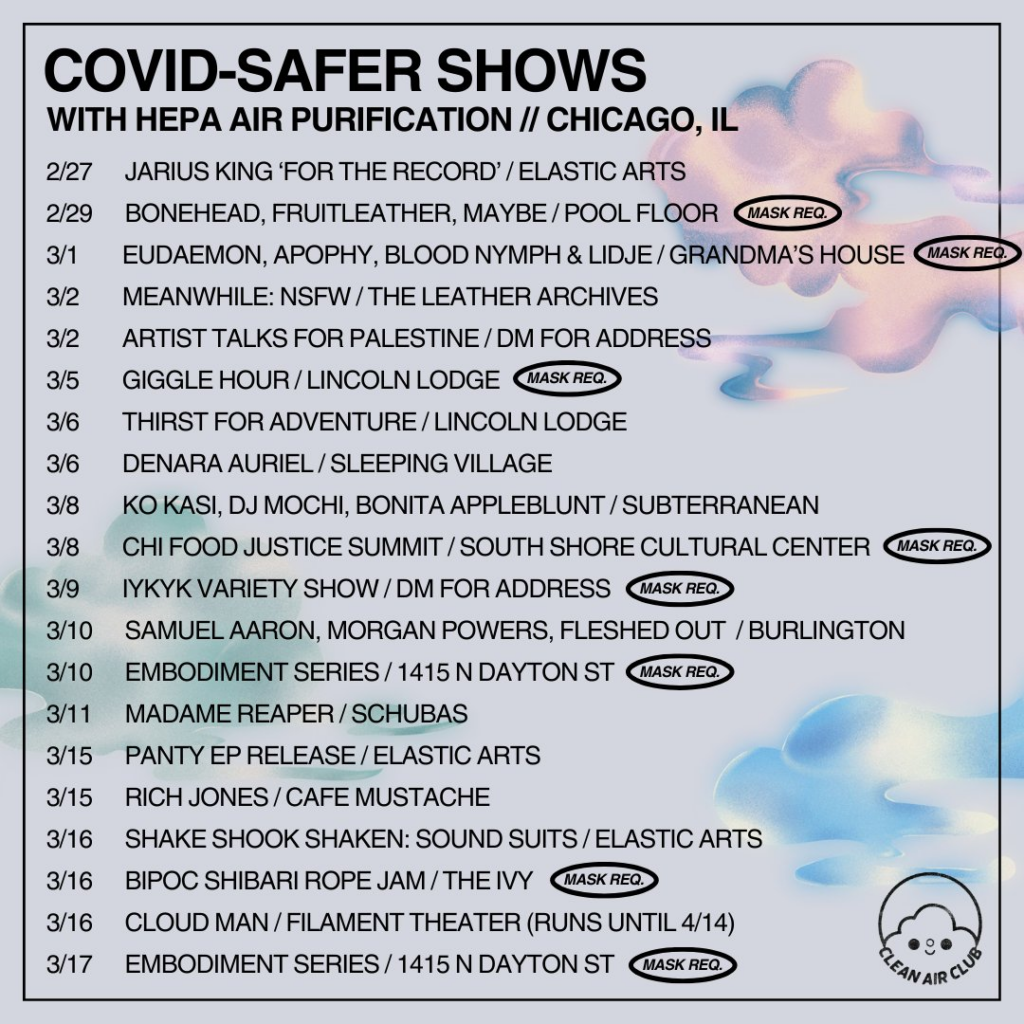
First, big acts could really help out smaller acts by supporting organizations like this one: [Clean Air Club]
Second, sell N95s at your concerts and on your websites as branded merch. K-Pop powerhouse Twice already does this (though KN94s, not N95s):
And if, by some happy chance, some intern from either organization reads this post, please champion these ideas!
Oh, and champion clean air, too. Who could be against that? Miasma delenda est!
Author(s): Lambert Strether
Publication Date: 28 Feb 2024
Publication Site: naked capitalism