Graphic:
Excerpt:
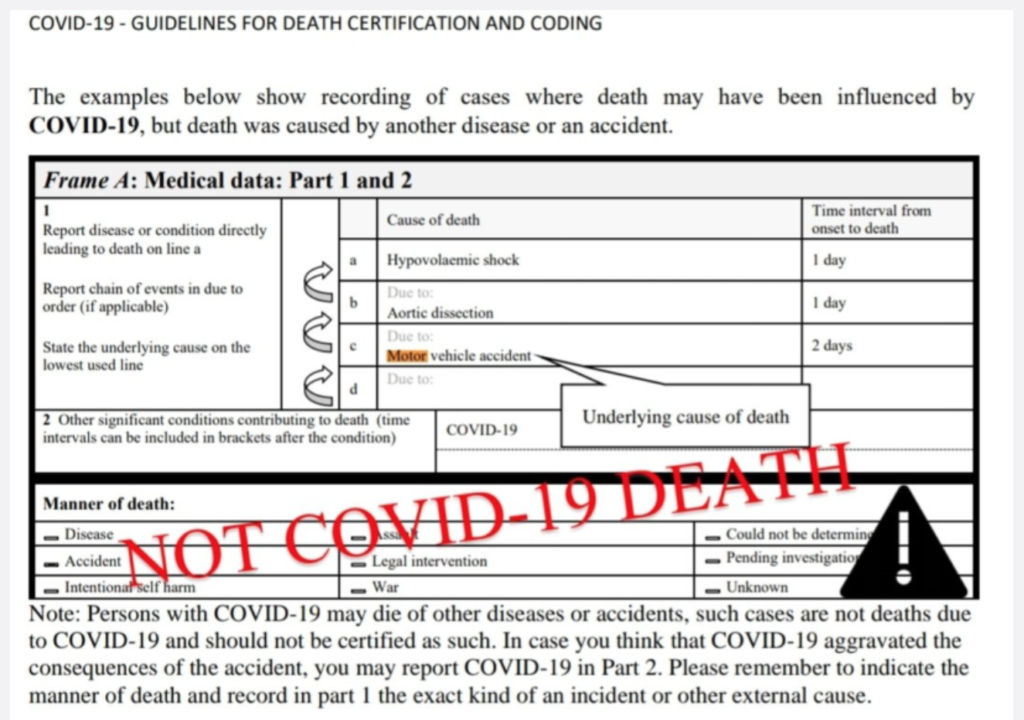
We had the opportunity to review death certificates for some of Florida’s recent COVID-19 deaths, and we can tell you definitively that Florida is counting deaths that were not directly caused by COVID-19.
Public health agencies have a goal of tracking the spread of a reportable disease, and for that reason, guidance was issued in March that any person who tested positive for COVID-19 should be counted as a COVID-19 death. However, the death count is now prominently featured in newscasts and used as a talking point to claim that some governments aren’t “doing enough” to stop the spread of COVID-19. COVID-19 metrics, including the number of reported deaths, are increasingly cited by governments as a reason to write public health recommendations into law.
……
A change in CDC guidance published on March 24, 2020 (COVID-19 Alert No.2) encouraged doctors to include COVID-19 in PART 1 “for all decedents where the disease caused or is assumed to have caused or contributed to death.” This was reinforced on April 5 (COVID-19 2020 Interim Case Definition), when the CDC said any death with COVID-19 on the death certificate is counted as a COVID-19 death, even if it was just presumed and had no confirming laboratory or clinical validation. In other words, the CDC guidance explicitly does not distinguish between deaths from COVID-19 and deaths with COVID-19.
This is contrary to World Health Organization (WHO) guidelines, which say to count only deaths “resulting from a clinically compatible illness, in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma). There should be no period of complete recovery from COVID-19 between illness and death. A death due to COVID-19 may not be attributed to another disease (e.g. cancer).”
Author(s): JENNIFER CABRERA AND LEN CABRERA
Publication Date: 11 November 2020
Publication Site: Rational Ground