Link: https://ijpds.org/article/view/1145
doi: 10.23889/ijpds.v5i1.1145
Graphic:
Excerpt:
Abstract
Introduction
More than 30 million adults are released from incarceration globally each year. Many experience complex physical and mental health problems, and are at markedly increased risk of preventable mortality. Despite this, evidence regarding the global epidemiology of mortality following release from incarceration is insufficient to inform the development of targeted, evidence-based responses. Many previous studies have suffered from inadequate power and poor precision, and even large studies have limited capacity to disaggregate data by specific causes of death, sub-populations or time since release to answer questions of clinical and public health relevance.
Objectives
To comprehensively document the incidence, timing, causes and risk factors for mortality in adults released from prison.
Methods
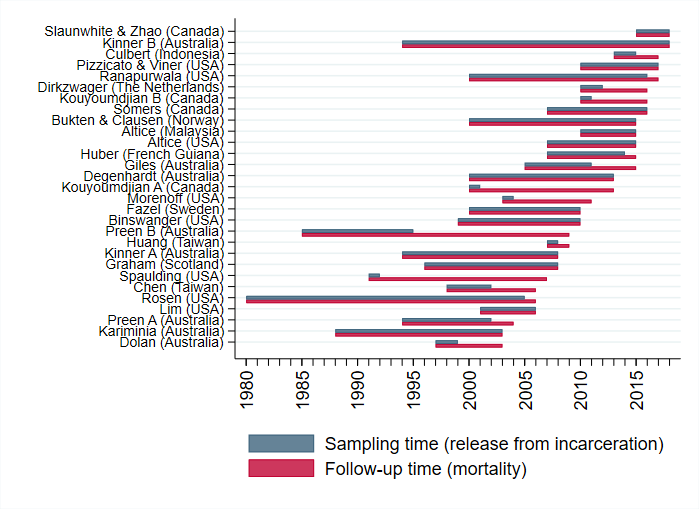
We created the Mortality After Release from Incarceration Consortium (MARIC), a multi-disciplinary collaboration representing 29 cohorts of adults who have experienced incarceration from 11 countries. Findings across cohorts will be analysed using a two-step, individual participant data meta-analysis methodology.
Results
The combined sample includes 1,337,993 individuals (89% male), with 75,795 deaths recorded over 9,191,393 person-years of follow-up.
Conclusions
The consortium represents an important advancement in the field, bringing international attention to this problem. It will provide internationally relevant evidence to guide policymakers and clinicians in reducing preventable deaths in this marginalized population.
Author(s): Borschmann, R., Tibble, H., Spittal, M. J., Preen, D., Pirkis, J., Larney, S., Rosen, D. L., Young, J. T., Love, A. D., Altice, F. L., Binswanger, I. A., Bukten, A., Butler, T., Chang, Z., Chen, C.-Y., Clausen, T., Christensen, P. B., Culbert, G. J., Degenhardt, L., Dirkzwager, A. J., Dolan, K., Fazel, S., Fischbacher, C., Giles, M., Graham, L., Harding, D., Huang, Y.-F., Huber, F., Karaminia, A., Kouyoumdjian, F. G., Lim, S., Møller, L., Moniruzzaman, A., Morenoff, J., O’Moore, E., Pizzicato, L. N., Pratt, D., Proescholdbell, S. F., Ranapurwala, S. I., Shanahan, M. E., Shaw, J., Slaunwhite, A., Somers, J. M., Spaulding, A. C., Stern, M. F., Viner, K. M., Wang, N., Willoughby, M., Zhao, B. and Kinner, S. A.
Publication Date: February 2020
Publication Site: International Journal of Population Data Science